Written By: Alexandra Heaney
As a Mental Health Nurse who spent many years working in a large metropolitan public mental health facility, I have seen my fair share of OVA. It’s interesting when I reflect on some of the things that occurred in my time there, and I often find when I talk about some of the more extreme things that happened, people are often shocked and horrified. I’ve been choked, spat on, shoved, and had glass shards thrown at me – and yet, none of these things were what impacted me the most long-term.
It was the everyday OVA, what we call ‘minor aggression’ – the insults, the arguing, the yelling – these were the things that took their toll the most. Perhaps because these are the things that occurred most often, but they were also the things that were overlooked the most when it came to the level of support you got from your team.
When something occurs so often as a part of your role, it starts to become embedded into the culture that that’s ‘just how it is’, or ‘you just need to be more resilient’, and over time, the care factor for the minor OVA is almost nil.
But what we know is that even during minor aggression, your amygdala still perceives the situation as a threat, your adrenaline and cortisol levels still rise, your fight or flight response still activates, and your body readies itself for an attack. This physiological response is the exact same as it is during a major OVA incident – your brain and your body literally cannot tell the difference between severity levels of OVA. So why should the support offered afterwards be any less?
In short, it shouldn’t be.
Activation of the Stress Response
- The brain’s amygdala perceives the situation as a potential threat and signals the hypothalamus to activate the sympathetic nervous system.
- This triggers the release of stress hormones, such as adrenaline (epinephrine) and cortisol, which prepare the body to respond.
- Heart rate and blood pressure rise.
(LeWine, H. E. (2024). Chief medical editor. Harvard Health Publishing)
Long-Term Impacts
If minor OVA incidents occur frequently or are not addressed, they can lead to:
- Chronic Stress: Repeated activation of the stress response.
- Burnout: Emotional exhaustion and reduced coping capacity.
- Heightened Sensitivity: Increased reactivity to future incidents.
(Department of Health, Victoria. (2018). Common reactions of people after OVA)
We work with a lot of clients who have front-facing staff experiencing OVA at all levels, but a large majority deal with minor aggression on a semi-regular basis. The difficult clients, the ones that yell at you for seemingly no reason, the ones that swear at you or call you names for just trying to do your job.
And yet the solution for most workplaces seems to be resilience training, EQ training and de-escalation training (all can be helpful of course), but there’s a major gap missing that isn’t being filled. Your post-incident response needs to be consistent, thorough, and above all – not contingent on the level of OVA that has occurred. All OVA is OVA.
What workplaces should be exploring is how do we train our leaders and our teams to respond after an OVA incident? How do we ensure that EVERYONE feels like they have the full support of their workplace behind them when something difficult happens? And how can we ensure we don’t become desensitized to OVA when it occurs so often in the modern world of work?
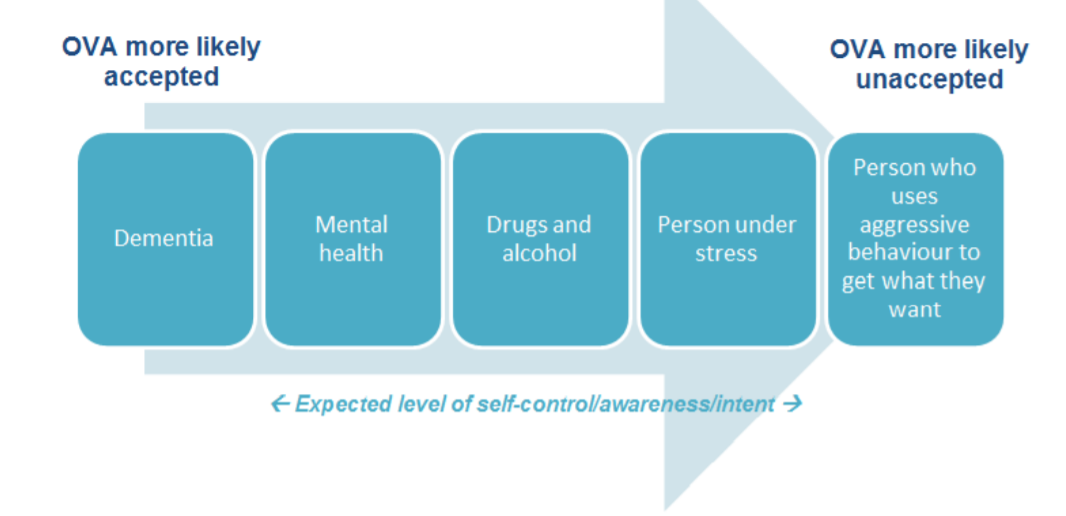
What we also know is that when organisations have a large client-base who are suffering from mental illness or are drug and alcohol affected, the level of acceptance for OVA rises even further. Why? Because we now have a reason for it. They’re not well, and so they don’t act well.
If a drug-affected person swears and yells at you at work – and this has become the norm, the response from teams and workplaces is often going to be even lower than it should be. And yet, if you’re dealing with this demographic, the OVA is likely to be more regular and sustained, which in turn causes higher burnout rates. Does this make sense to you? Don’t worry, it doesn’t make sense to me either!
After working in this space for so long, I can tell you there’s no magic wand to fix OVA. It is a part of work life for many of us, even if we wish it wasn’t – people are complex beings.
What I can also tell you is that the support your leaders and team provide each other during and after an OVA incident (regardless of severity) will be crucial for promoting emotional recovery, rebuilding trust and ensuring the mental wellbeing of all employees at work.
Ways You Can Support a Colleague Post-Incident 👇
- Check-In: Ask if they are okay as soon as you can after the incident. This shows them that you are aware that it happened, and you care about their wellbeing.
- Ask What They Need: Some people may want to talk, while others may prefer quiet time. Offer support in a way that aligns with their preferences.
- Listen Without Judgment: Allow them to express their feelings or recount the incident without interrupting or downplaying their experience.
- Offer Small Gestures of Care: Simple actions, like checking in with a warm smile, putting a hand on their shoulder or inviting them for a coffee break, can make a big difference.
- Acknowledge Their Experience: Validate their feelings by saying things like, “That must have been really difficult” or “It’s okay to feel upset.”
- Avoid Forcing a Discussion: If they’re not ready to talk, let them know you’re available when they are.
- Assist with Reporting the Incident: Offer to help them complete any necessary incident reports or paperwork.
- Support Workload Adjustments: Coordinate with your team or supervisor to lighten their responsibilities if needed.
- Check in Regularly: In the days and weeks following the incident, ask how they’re doing and if there’s anything they need. This is particularly helpful for those who may have lingering affects but don’t want to appear ‘weak’ or burden anyone.
- Monitor for Signs of Distress: Be aware of changes in their mood, behaviour, or performance that may indicate ongoing stress or trauma.
- Be Patient: Recovery takes time, and their needs may change as they process the event.
If you’d like to learn more about post-incident support for your leaders or teams; get in touch at alexandra@tanyaheaneyvoogt.com.
Remember; all OVA is OVA.
Al
About Alexandra Heaney
Certified Clifton Strengths Coach, Resilience Coach & Associate Consultant
Alexandra (Al) is a Gippsland-based Clifton Strengths Coach, Resilience Coach and Associate Consultant for Tanya Heaney-Voogt.
Passionate about creating positive workplace change and improving workplace culture, Al has a rich history to draw from to achieve these goals.

With a career spanning 5 years as a Psychiatric Nurse at the Alfred Hospital Acute Inpatient Unit, 2 Years of Studying Psychological Science, and a current degree in progress in Counselling, human behaviour and positive psychology have always been concepts she is passionate about.
Her ability to integrate this knowledge into meaningful and insightful discussion regarding the Clifton Strengths assessment and general workplace challenges makes her a proficient guide for coaching clients.
Al is adept at empowering others to pursue their objectives by consciously harnessing their innate talents and strengths.
In her spare time, Alex is also a passionate reader and film enthusiast, and enjoys spending time with her partner Kevin and their fur baby (puppy) Homer.
If you’d like to learn more about your Strengths or find out more about Al’s coaching and consulting services; email Al for more information at:


Recent Comments